Chronic Pain Explained
What is it and why is cure so difficult?
In this article we provide a simple overview of Chronic Pain, its origins, why it is so complicated and why it is so difficult to cure. Throughout the article we provide links to useful resources, with further information on Chronic Pain, the many factors that contribute to the pain experience, and to further articles on best practice treatment.
As an example, the following short video from the NZ Faculty of Pain Medicine provides a useful overview of Chronic Pain & its treatment. The video describes how Chronic Pain affects a significant portion of the population, the complicated nature of Chronic Pain, the expertise required to assess & treat the condition, the many aspects of effective treatment & how it may take some time to start feeling better.
What is Chronic Pain?
Chronic or Persistent pain is an extremely common condition, which affects 20% of the population to varying degrees. So while you may feel frustrated, misunderstood or isolated with your experience of Pain, you are not alone, as 1 in 5 people have a Pain experience somewhat similar to your own.
There are generally two types of pain, these are Acute Pain and Chronic Pain.
Acute Pain lasts for a short amount of time, and occurs following physical damage to body tissue. Acute pain serves the purpose of alerting you to some form of physical danger and getting you to take protective action to remove the cause of pain - it acts as an alarm system. Once the damaged tissue heals it is usually found the pain will disappear.
Chronic Pain on the other hand, is not necessarily associated with active disease and/or physical tissue damage as a result of an injury. Many people report this type of pain in the absence of tissue damage or any likely pathophysiological cause. The NZ Pain Society (NZPS) talks about Chronic Pain sticking around long after the body has healed, or even when there was very little damage. They indicate that Chronic Pain can result when the alarm system becomes over sensitive. The NZPS have a patient booklet describing Chronic Pain, how it may feel & impact on your life, and some guidance on how to navigate you way through Chronic Pain
Obtaining a strict definition for Chronic Pain is somewhat difficult due to its complexity and the many factors that influence the pain experience. The technical definition for Chronic pain describes it as “Continuous long-term pain of more than 12 weeks or that persists beyond the expected period of healing after trauma or surgery”.
One of the defining characteristics of chronic pain is that it is ongoing and experienced on most days of the week. However, how do we define Pain itself? The IASP (International Society for the Study of Pain), in its updated definition, defines pain as, “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”.
By talking of the sensory and emotional experience, the IASP definition starts to recognise pain as a personal experience, and one where the “same” amount of tissue damage can feel quite different to different people. Because it is a sensory & emotional experience, it cannot be measured exactly with something like a “pain thermometer”. Chronic pain is not an exact thing, it is a name used to describe a collective multitude of pain experiences, which are highly variable and uncertain in their nature, and that emerge from the incomprehensible system that is the human body.
Chronic pain is now also recognised as a disease in its own right, rather than being a symptom of some other active disease. The different forms of Chronic Pain now have their own World Health Organisation (WHO) International Disease Classifications Codes (ICD).
If Acute Pain is thought of as helpful pain, then Chronic Pain is often thought of as unhelpful pain, due to it being much more difficult to understand, treat & get through. As indicated in the above short video, Chronic Pain often starts to seep into and impact other parts of your life. At times, this impact can be so great that Chronic Pain, and associated emotional conditions such as depression, have all been referred to as “cancer of the soul”.
Based on all the above, Chronic Pain tends to:
- Persist for longer than 3 months & after normal tissue healing has taken place - it is ongoing & experienced for most days of the week.
- Be unable to be explained by some other primary diagnosis (e.g. active disease or injury)
- Be associated with significant emotional stress & functional disability
In the following sections we start to explore the many factors that contribute to the Chronic Pain experience and why it is so complicated.
What is the Origin of Chronic Pain?
In some cases, the original origin of Chronic Pain is some physical cause, such as injury, surgery, musculoskeletal conditions such as arthritis, or other medical conditions such as cancer, endometriosis or migraines. However, in some cases, there may be no apparent physical cause.
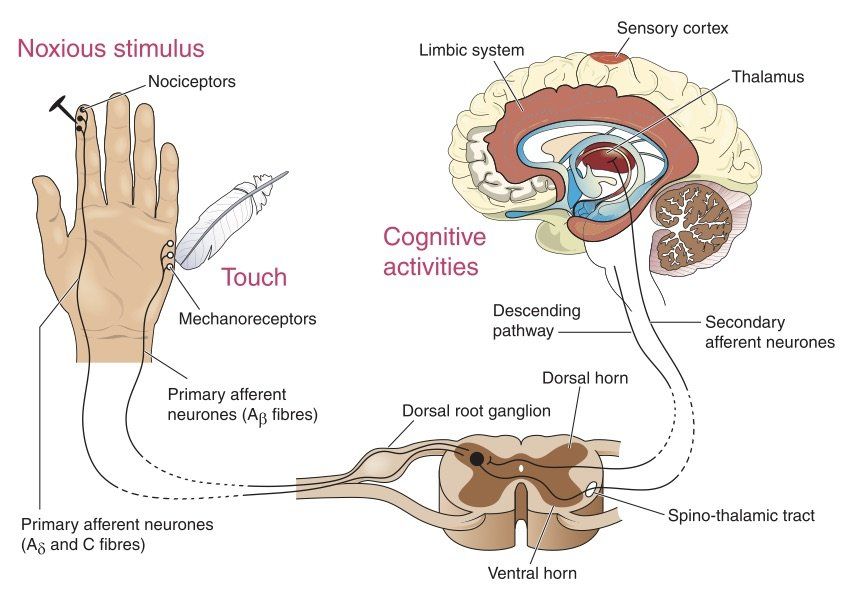
Even when the origin is physical, the feeling of pain does not have its origin in the damaged tissue, but in the nervous system's response to, and attempt to protect us from, the cause of the damage. This is why it is important to treat acute pain quickly, as under treated acute pain, can result in a sensitised nervous system, and develop into Chronic Pain.
Pain Australia have produced a useful 2-page fact sheet on The Nature & Science of Pain. It describes the three neurobiological mechanisms that are the foundation of pain. These are:
- Nociceptive Pain, which originates in specific nerves located in the body’s tissues known as Nociceptors. It is the type of pain you would usually experience as a result of an injury, and is often described as a sharp, aching or throbbing pain. When the tissue where these nerves are located is damaged, these Nociceptive nerves send signals via the spinal cord to the Brain. If the Brain interprets these signals as dangerous, it will then create the pain sensation to warn us about, & protect us from, whatever has damaged the tissue. The Brain regulates the pain sensation based on our previous experiences and the level of threat to us.
- Neuropathic Pain, has its origins in damage to the neural tissue in the nervous system itself. This type of pain has many causes, but almost all are related to some some active disease or medical intervention, such as viral infections, shingles, multiple sclerosis, diabetes, stroke, alcoholism, surgery, amputation & compression of nerves. The pain is often described as burning or shooting pain, and the skin can be numb, tingling or extremely sensitive to even mild stimuli such as a breeze or a light touch.
- Nociplastic Pain, has its origins in how sensory neurons function. While it is similar in nature to neuropathic pain, it comes about when neurons become more responsive (sensitive) to stimuli rather than from direct nervous system damage.
Acute pain is typically Nociceptive, but can also be Neuropathic. Chronic Pain typically has Neuropathic and Nociplastic components, and can have a Nociceptive component. It can be seen from the above discussion that the nervous system has a pain ‘memory’ and ability to rewire itself in response to pain (i.e. neuroplasticity). It is this pain memory that leads to pain sensitisation and often Chronic pain
While Biophysical factors, such as pain memory and sensitisation, have a significant role to play in a person’s Chronic Pain experience, there are also other factors that modulate how a person experiences and manages Chronic Pain. That is, Chronic Pain is often even more complicated than described above, and we discuss the additional factors in the next section
Why is Chronic Pain so Complicated?
On a biophysical level, pain is complicated because it is not simply a feeling produced within the tissue due to damage of that tissue. It is the response of another rather complicated system, the nervous system, to that damage.
The complication is increased by the Nervous system’s ability to adapt to and remember the pain experience. This ability to regulate or modulate the pain experience can be useful, when the system turns down the experience of pain. However, in the case of Chronic pain, the nervous system often becomes oversensitised and amplifies & prolongs the pain experience.
If these direct biophysical factors are not complicated enough, the development & experience of chronic pain is further modified by other factors in a person's life. These additional factors are Psychological, Social and indirect Biophysical factors. This understanding of the additional factors, and how they influence a person’s pain experience, has led to the Biopsychosocial or Sociopsychobiomedical model of pain. Thus, Chronic pain should not simply be treated as a biophysical problem, but it must be assessed, diagnosed, treated and managed through consideration of all three aspects of the Sociopsychobiomedical model. This approach considers the whole person and their experience of pain.
Examples of factors that could exist, within each area of the Sociopsychobiomedical model of pain, and influence a person’s pain experience, are:
- Social factors, such as the response of other people at home and at work to the person’s pain and the impact it is having on their life. If a person is criticised, unsupported, and attitudes & beliefs exist that undermine the reality of the condition, then a person’s pain experience will tend to be worse than in a supported environment. Social factors can also include financial health and access to health-care.
- Psychological factors, such as anxiety, depression, fear & guilt. If a person thinks much about their pain, thinks it is worse than it is, is anxious about how it is impacting them & their family, and feels helpless to manage it, the pain experience will tend to be worse. Conversely, if they are preoccupied with other activities & distracted from the pain, this will decrease pain intensity.
- Indirect Biomedical factors, such as whether the person has other illnesses or factors that influence pain sensitivity and thresholds. This could include, sex & stress hormone levels. The direct biophysical factors are those associated directly with the nervous system response.
The many factors described above, which influence a person’s Chronic pain experience, are probably now starting to make it evident as to why Chronic Pain is so difficult to cure, and why a silver bullet cure often does not exist. In the next section we describe some of the factors that make finding a simple cure for Chronic Pain so elusive.
Why is Chronic Pain so Difficult to Cure?
If we start to think about the nature of Chronic pain, we can begin to understand why Chronic Pain is so difficult to cure. Some of the aspects that make Chronic pain so difficult to cure are:
- Chronic pain is a multifaceted health issue and as such is likely to require a multifaceted treatment strategy
- The systems within the human body that are responsible for producing and modulating the pain experience are complicated or complex systems, and as such the assessment and treatment of pain is also likely to be complex
- With time the nervous system continues to modulate the pain experience, and so there can be an aspect of chasing a moving target. This is why it is so important to seek treatment for pain in a timely manner, however this is often hindered by the condition's complexity obscuring where best to send the person for assessment & treatment.
- The Sociopsychobiomedical model of pain, means there are some aspects influencing your chronic pain experience that are out of your control, however, what will be required is management or coping strategies to deal with these adverse external influences.
- The complex and Sociopsychobiomedical nature of Chronic Pain means no individual health professional will have the training required to undertake all aspects of your treatment. For this reason it has been found that interdisciplinary teams, consisting of a Pain Specialist, Physiotherapist, Psychologist, Occupational Therapist & others, provide the most effective treatment.
- Understanding all there is to understand about Chronic Pain, and effectively assess and treat Chronic Pain, requires specialist knowledge. For this reason, those who have particularly complex Chronic Pain are often referred to a Pain specialist. Many non-specialist Medical Professionals find it a challenge to understand Chronic Pain and say they are not confident in assessing & treating Chronic Pain.
Given all the above we can now start to understand why Chronic Pain is so difficult to cure, why specialist knowledge maybe required to treat the condition and why relief from the condition may take some time. The Faculty of Pain Medicine Video at the start of this article, serves as a useful reminder of all these aspects of Chronic Pain.
The Australis Specialist Pain Clinic (ASPC) has within its team a number of pain specialist who are qualified & experienced in assessing & treating the complex condition that is Chronic Pain. ASPC offers best practice care by using the Sociopsychobiomedical model of pain and interdisciplinary teams.
In follow on articles in this series, we explore in more detail a number of key aspects introduced in this article. This includes, articles that:
- Describe how pain is an output of the brain, and provides some interesting examples showing how sometimes our brain can trick all of us.
- Provide an overview of what is currently considered to be Best Practice in Chronic Pain assessment & Treatment
- Describe the evidence supporting the Interdisciplinary Team approach, and give an overview of all those clinicians who maybe part of this team and why.